South Australian Medical Heritage Society Inc
Website for the Virtual Museum
Home
Coming meetings
Past meetings
About the Society
Main Galleries
Medicine
Surgery
Anaesthesia
X-rays
Hospitals,other organisations
Individuals of note
Small Galleries
Ethnic medicine
- Aboriginal
- Chinese
- Mediterran
Diathermy and Electro-Surgery
ACKNOWLEDGEMENTS
We are most grateful to Jan Hooper of the TQEH History Museum and the theatre staff for allowing us to photograph their items.
The attraction of hair and small pieces of paper to a rubbed ebony rod has been known by the Egyptians and others for at least two millennia, but electricity was not studied until the last 3 centuries. Although English and American inventors are frequently quoted, other nations were also individually involved.
Benjamin Franklin (1706-1790) is known for his lightning experiments and coining the words positive and negative charges.
Thomas Alva Edison (1847-1931) is reputed for inventing the first commercially practical electric light globe in 1879.
George Westinghouse (1846-1914) started to generate electricity using water turbines at Niagara Falls and transport it by wire as an alternating current in 1895.
Nikola Tesla (1856-1943) convinced the Americans that alternating current was a better means of distribution. He also proposed that various current frequencies had different tissue effects and may have suggested a medical use.
Heinrich Hertz (1857-1894) studied and confirmed the presence of electromagnetic waves. His name is given to the unit which measures their frequency.
DIATHERMY
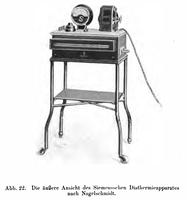
The word diathermy, which means "heating through" (from the Greek words "dia" "through", "across" and "thermē" "heat"), refers to the production of heat by passing a high frequency current through tissue. It was coined in 1908 by German Physician Karl Franz Nagelschmidt, one of the founders of diathermy, who literally wrote the book on it ("Lehrbuch der Diathermie für Ärzte und Studierende", "Diathermy Textbook for physicians and students", 1913).
His book names the several Hertz wave frequencies, and suggests their optimal use for haemostasis and tissue resection. The short wave diathermy has different Hertz values, and these vary with the specific intended uses, such as bipolar, harmonic, or unipolar modes.
In the medieval ages haemostasis was sometimes achieved by red hot stones or irons applied to the bleeding surface, a heroic and risky procedure.
More recently, cautery using a 240 volt power source to heat the probe tip was used to remove cervical erosions. It was effective and achieved good haemostasis, but the cells were destroyed and histological diagnosis was not possible. A preliminary biopsy was needed.
-
 A unipolar diathermy machine from ~1900s. Source: Wellcome Images
A unipolar diathermy machine from ~1900s. Source: Wellcome Images -
 Short wave bipolar diathermy machine from 1933.
Short wave bipolar diathermy machine from 1933.
Source: Wikipedia

Some current machines at the QEH are shown below. They have unipolar and bipolar settings. The frequencies can be changed, and a harmonic mode is available. They provide the possibility of bloodless tonsilectomy if the correct plane of tissue is used. Their use make laparoscopic sugery possible.
Appendix
In medicine, there are three main techniques used in diathermy: ultrasonic, shortwave ( ~1 - 100 MHz ) and microwave ( ~300 MHz - 300 GHz ). They all cause tissues to heat up, which can be used to, for example, relax muscles, assist physical therapy, cut, or cauterise. This section focuses on the electromagnetic surgical forms only.
There are two branches of electrical diathermy: electrocautery and electrosurgery.
Electrocautery
Electrocautery passes a DC through a loop, which then becomes hot due to resistance, allowing the surgeon to burn away tissue and cauterise the wound at the same time. This current does not enter the patients body, and the tissues are damaged via thermal condution. This is much the same as cauterising with a hot knife, or destroying tissue with a burning stick.
One early application was by the French surgeon and gynaecologist Joseph C. A. Recamier, who from around 1830 used electrocautery to treat uterine cancers. In 1874, the Piedmontese (now a part of Italy) surgeon Enrico Bottini created a device for "cauterio termogalvanico" ("thermo-galvanic cautery") to treat prostate cancer.
Electrosurgery
In electrosurgery, an AC passes through the patient, resulting in dielectric heating of the tissue, the same effect as in a kitchen microwave oven. Typically, electrosurgery uses AC frequencies of 200 kHz - 3.3 MHz, as nerve and muscles stop responding to stimulation at around 100 kHz.
Around 1881, the heating effects of high frequency currents started gaining attention. Nikola Tesla noted these effects, and suggested that they may have medical uses. About the same time, the French biophysicist Jacques Arsene d'Arsonval was conducting tests, including subjecting himself to a high frequency 3 Ampere current, noting there was no electric shock, only heat.
d'Arsonval's devices became popular, and he treated several people in the 1890's, for a wide range of ailments, including circulatory disorders, skin diseases, and tuberculosis.
In 1907, Karl Nagelschmidt demonstrated that high frequency currents could heat deep tissue, and could be used to treat joint problems.
Better generators were developed from ~1910, allowing diathermy to be used surgically. These were grounded through the wall, but could easily be grounded through many other less desirable paths, such as the patient, or the operators. It wasn't until 1968 that isolated generators were developed, greately reducing these problems.
Dr William T Bovie created a diathermy machine in 1926, which was first used on the 1st of October, 1926, by Dr Harvey Cushing to remove a mass from his patient's head, and was well pleased by the lack of bleeding.
The use of microwave frequencies was suggested in 1938-39 by H E Hollman, and came into use by the 1950's.
The next significant improvement came in the 1990's, with active monitoring of the current. Return electrode monitoring was added, which allowed the generator to adjust its output, depending on the impedance of the return electrode pad, which is proportional to the area of the pad touching the patient. This significantly reduced the likelyhood of burns at the return electrode.
There are two main types of electrosurgery: monopolar and bipolar. As the name suggests, the bipolar form uses two poles, an active and a return, at the surgical site. This limits the current to flowing between the two electrodes. In the more common monopolar form, the surgeon works with the active probe, and the current flows through the patient, exiting through the patient return electrode (similar to a grounding pad) placed near the operating site on well vasculated, non-boney areas, eg: the thigh or buttock. This can result in burns if the pad does not make good contact with the patient.
Electrosurgery works by using the current to heat tissue, described by Joule's law, E = (IRMS)2 x Re(Z) x t, where E is the energy (heat), IRMS is the root mean square of the current, Re(Z) is the real component of the impedance, and t is time. The more heat produced, the more tissue is damaged. The amount of heat can be varied by changing the duty cycle (the time "on" during each period of the waveform), or increasing the voltage. This allows the surgeon to "cut", coagulate, or dessicate tissue.
Tissue can be dessicated when the electrode contacts the tissue. This prevents sparking, and causes the tissue to heat.
Cutting is achieved by holding the electrode slightly away from the tissue, resulting in small arcs. This very rapidly heats a small area, causing the tissue to quickly vapourise, and the cells to explode.
Coagulation can also be done by fulguration. This is when the coagulation waveform (low duty cycle, and often a higher voltage) is passed through the electrode, which is held further away from the site. This allows the charge to dissapate over a larger area, further reducing the heat, preventing the cutting action.
Both the coagulating and cutting waveforms result in coagulation by heating the tissue, with the cutting waveform affecting a larger volume than the coagulating waveform.
A "blended cut" mode is a mixture of cutting and coagulating. By reducing the duty cycle of the waveform, one can reduce the amount of heat produced, changing the relative proportion of cutting to coagulating.
More recently, lasers have also been used for cutting and coagulation, espescially in the delicate eye.
As electrosurgery can produce significant heat, care must be taken to avoid fires. Flammable alcohol-based skin preparation fluids should be allowed to dry completely before surgery, and combustible material (preparation fluid containers, swabs, hair, etc) should be kept away from live diathermy tools.
Diathermic surgery has become a very commonly used and safe technique, and is used in many fields of medicine. The reduction in bleeding allows for more difficult areas (eg: endoscopic surgeries, highly vascularised masses, etc) to be treated safely, improving the lives of many.